Updated October 16, 2020
Issue/Situation
The CDC and other public health agencies are monitoring a respiratory illness outbreak caused by a novel coronavirus. The new coronavirus was first identified in Wuhan, Hubei Province, China and has caused illnesses throughout China and around the world, including in the United States.
The virus has been named “SARS-CoV-2” and the disease it causes has been named “coronavirus disease 2019” (abbreviated “COVID-19”).
Background Information
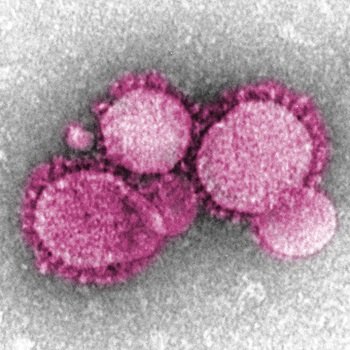
What is the coronavirus?
The 2019 novel coronavirus is from a family of viruses known as coronaviruses that are common around the world. Coronaviruses are found in different animals such as camels, cattle, cats and bats and some coronaviruses can infect people.[1] The 2019 novel coronavirus is a new strain of the virus that has not previously been identified in humans. Human coronavirus can cause mild to moderate illness; however, some of the newer human coronaviruses can cause severe illness, even death. [2] Examples of other human coronaviruses that have caused severe illness in the past include the coronavirus that causes Middle East Respiratory Syndrome (MERS) and the coronavirus that causes severe acute respiratory syndrome (SARS).
How is the coronavirus transmitted?
The initial patients were linked to a seafood and animal market suggesting that the virus was spread from animal to person. However, a large number of patients were not exposed to an animal market which indicates that the virus is spreading from person to person. It is thought that the virus is spread person-to-person through the respiratory droplets when an infected person coughs or sneezes.
What are the symptoms of the coronavirus?
Individuals infected with COVID-19 have had mild to severe respiratory illness with symptoms ranging from little to no symptoms to severe. Symptoms include fever, cough, shortness of breath, chills, difficulty breathing, fatigue, muscle or body aches, headache, new loss of taste or smell, sore throat, congestion or runny nose, nausea or vomiting and diarrhea. In more severe cases, symptoms include pneumonia, severe acute respiratory syndrome, kidney failure and even death. Typically, symptoms appear 2-14 days after exposure to the virus. [3]
What can be done to prevent the spread of coronavirus?
The virus is thought to spread from person-to-person. General precautions should be taken to prevent the spread of infection such as frequent handwashing, covering mouth and nose with a cloth face covering when around others, covering mouth/nose when sneezing, avoiding close contact with anyone experiencing respiratory illness symptoms such as coughing and sneezing and cleaning and disinfecting frequently touched surfaces. [4]
Coronavirus and Food
Can a person contract coronavirus from food?
Coronavirus is a respiratory virus spread through respiratory droplets. The Centers for Disease Control and Prevention (CDC) does not consider COVID-19 to be a foodborne illness, but similar actions to prevent foodborne illness can be taken to mitigate the spread of COVID-19. The most important actions to take include proper handwashing using soap and water and scrubbing for at least 20 seconds, frequent cleaning and sanitation of touch points and staying home when sick or caring for someone who is sick.
Can food packages or food products help spread the virus?
Currently, there is no evidence that the transmission of COVID-19 is associated with food or food packaging. Unlike foodborne gastrointestinal (GI) viruses like norovirus and hepatitis A that often make people ill through contaminated food, SARS-CoV-2, which causes COVID-19, is a virus that causes respiratory illness. Foodborne exposure to this virus is not known to be a route of transmission. The virus is thought to spread mainly from person-to-person. This includes between people who are in close contact with one another (within about 6 feet), and through respiratory droplets produced when an infected person coughs or sneezes. These droplets can land in the mouths, eyes or noses of people who are nearby or possibly be inhaled into the lungs. It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads. However, it’s always critical to follow the 4 key steps of food safety—clean, separate, cook, and chill – to prevent foodborne illness. [5]
Can reusable bags transmit coronavirus?
While there is a lack of evidence that reusable bags can be a vehicle for transmitting the coronavirus, reusable bags and totes can become unsanitary and a vehicle for cross contamination if not properly cared for. The CDC recommends cleaning and disinfection as a best practice measure for prevention of COVID-19 other viral respiratory illnesses. In addition, cleaning and disinfecting reusable bags is essential for food safety. Retailers can encourage customers to take the following preventive actions:
- Use a clean grocery bag (reusable, plastic or paper) or tote.
- Use dedicated totes and bags only for groceries.
- Wash reusable bags and totes after each use.
- Always follow cleaning instructions provided on reusable bags.
- Store bags and totes in a clean, cool and dry location and do not store in garage or in car.
- Keep raw products like meat and poultry away from ready-to-eat foods (e.g., using separate bags for raw and ready-to-eat foods).
- Use separate reusable bags for food items and non-food items (e.g., household cleaners, detergents, etc.).
Additional Reusable Bag Resources:
- NC State Cleaning and Disinfecting Reusable Bags
- Cleaning Institute Guide for Cleaning Reusable Bags
- CA Department of Public Health Practical Tips For The Use And Care Of Reusable Grocery Shopping Bags
Partnership for Food Safety Education Retailer Resources:
- Don’t Wing It – Support customers in reducing the risk of foodborne illness for themselves and their families by promoting safe handling of raw meat to reduce the risk of cross contamination.
- ProducePro – Educate customers to become ProducePros and give them the knowledge they need to consistently practice basic safe handling and hand hygiene when preparing fresh produce at home.
Employee and Customer Health and Safety
What actions should food establishments take?
Food establishments should ensure that they have strong food safety programs in place and ensure employees are washing hands properly, practicing good personal hygiene, avoiding bare hand contact with ready-to-eat foods, staying home when sick, and are following proper cleaning and sanitation procedures. [6]
Employee health policies should be re-examined and updated to ensure ill food workers are excluded from working in a food establishment. Allow for flexibility with work conditions in order to encourage employees with symptoms, as well as family members/caregivers with symptoms, to stay at home.
What are grocery stores doing to protect customers from coronavirus?
Grocery stores have the health of their customers in mind every day. CDC recommends that grocery stores continue to practice routine cleaning and disinfection, especially on surfaces that are frequently touched by multiple people, such as door handles, desks, buttons, carts and touch screens, etc. The frequency of cleaning and disinfecting that is required is based on the level of use. CDC has published a FAQ, which is available here, on cleaning and disinfection that they are continually updating. Food retailers should continue to use cleaners and disinfectants according to label instructions and leverage EPA-registered cleaning and disinfecting products that are already on the market.
How are food retailers and product suppliers protecting their workers?
Food retailers and product suppliers are unique in that they both serve and employ so many of their consumers in neighborhoods. If a worker is sick, their health is the priority. Many companies have deployed new emergency leave policies for their workers in affected areas. Related, the major insurance providers have extended the request from the White House to alleviate cost burdens related to COVID-19 visits.
www.FeedingUS.org has several joint documents from the food and beverage industry including guidance on physical distancing in manufacturing facilities.
Should employees or customers wear face masks?
The CDC recommends that individuals wear masks in public settings, especially in areas where other social distancing measures may be difficult to maintain (e.g., grocery stores and pharmacies).The masks that the CDC recommends include do not include the N95 respirators which are critical supplies that must continue to be reserved for healthcare workers and other medical first responders. It is important to note that wearing a face mask is not a substitute for social distancing and individuals should try to keep a 6-foot distance between one another when possible.
Studies show that individuals can transmit the virus to others even when they aren’t showing symptoms (i.e., asymptomatic) of being infected with coronavirus. Wearing a mask can act as a barrier to protect against droplets, for example, from speaking, coughing, sneezing, and help prevent the spread between people who are in close proximity, even if those people are not exhibiting symptoms. Masks work best when everyone wears them.
Masks should always be worn as they are intended. Correct and consistent mask use is a critical step everyone can take to prevent getting and spreading COVID-19. Individuals wearing masks should continue practicing good personal hygiene and wash their hands before putting on a mask, after taking off mask, and after touching/adjusting the mask.
Employees working in a grocery store who wear a cloth face covering should launder their reusable face covering before each daily use as well as maintain their face covering according to Sections 4-801.11 Clean Linens and 4.802.11 Specifications of the FDA Food Code. Whether or not an individual chooses to wear a mask, everyone must continue to follow all safe practices to prevent the spread of COVID-19. Additional information is available from the World Health Organization on when and how to use a mask.
What are the CDC's recommendations on wearing double masks?
There are many types of masks that can be used to prevent getting and spreading COVID-19 and there are pros and cons for different masks. On February 10, 2021, CDC updated its mask guidance, reemphasizing that correct and consistent mask use is critical in the prevention of getting and spreading COVID-19. The updated guidance focuses on the importance of fit, filtering ability and layers of material when choosing a mask and provides various ways of improving mask protection.
CDC’s guidance does not exclusively recommend double masking as a new standard; rather, the guidance mentions wearing a disposable mask underneath a cloth mask as one of the many ways to enhance mask performance. Furthermore, CDC states that neither combining two disposable masks nor combining a KN95 mask with any other mask are not effective easy for improving fit and enhancing mask performance. In addition, CDC suggests knotting and tucking the ear loops of a medical mask and then tucking in and flattening the extra material close to the face as another way to improve the fit of a mask.
Although use of double masking (i.e., disposable mask under cloth mask) or knotting and tucking are two of many options that can optimize fit and enhance mask performance for source control and for wearer protection, double masking might impede breathing or obstruct peripheral vision for some wearers, and knotting and tucking can change the shape of the mask such that it no longer covers fully both the nose and the mouth of persons with larger faces.
The updated guidance is based on a recent CDC study which demonstrated the importance of good fit to maximize mask performance. CDC’s updated guidance on masks is available here. Additionally, the publication, Maximizing Fit for Cloth and Medical Procedure Masks to Improve Performance and Reduce SARS-CoV-2 Transmission and Exposure, 2021, that provides the supporting science is available here.
What happens if a grocery associate is identified to have COVID-19?
The food industry is a part of our nation’s “critical infrastructure” and must remain operational to feed the country. If an employee is diagnosed with COVID-19, physicians work with state or local health departments, and public health personnel will follow up to interview and assess these individuals. A store will also work with its local health department to determine the best course of action since there will be variability depending on the level of community spread in the given area. Importantly, the associate will be asked to stay home and not return to work until they are asymptomatic and meet the CDC guidelines along with any state/local health department requirements for returning to work. For specific protocols that a company in the food industry should take if an employee or customer tests positive for COVID-19, visit: https://www.feedingus.org/.
Can I take an employee's temperature at work to determine whether they might be infected and what precautions are needed for individuals who are taking the temperatures?
Yes. The EEOC confirmed that measuring employees’ body temperatures is permissible given the current circumstances. While the Americans with Disabilities Act (ADA) places restrictions on the inquiries that an employer can make into an employee’s medical status, and the EEOC considers taking an employee’s temperature to be a “medical examination” under the ADA, the federal agency recognizes the need for this action now because the CDC and state/local health authorities have acknowledged community spread of COVID-19 and issued attendant precautions.
However, as a practical matter, an employee may be infected with the COVID-19 coronavirus without exhibiting recognized symptoms such as a fever, so temperature checks may not be the most effective method for protecting your workforce. Note: If your company does business in the State of California (e.g., if you have one or more locations, employees, customers, suppliers, etc. in the state), and your business is subject to the California Consumer Privacy Act (CCPA), then you must provide employees a CCPA-compliant notice prior to or at the same time as your collection of this information. For advice on CCPA compliance, please reach out to any member of our Data Security and Workplace Privacy Practice Group at any of California offices.
To protect the individual who is taking the temperature, you must first conduct an evaluation of reasonably anticipated hazards and assess the risk to which the individual may be exposed. The safest thing to do would be to assume the testers are going to potentially be exposed to someone who is infected who may cough or sneeze during their interaction. Based on that anticipated exposure, you must then determine what mitigation efforts can be taken to protect the employee by eliminating or minimizing the hazard, including personal protective equipment (PPE). Different types of devices can take temperature without exposure to bodily fluids. Further, the tester could have a face shield in case someone sneezes or coughs. Further information can be found at OSHA’s website, examining the guidance it provides for healthcare employees (which includes recommendations on gowns, gloves, approved N95 respirators, and eye/face protection).
For additional information see Fischer Phillips FAQs For Employers On The COVID-19 Coronavirus.
When can employees return to work after a diagnosis of COVID-19?
According to CDC guidelines:
- Employees can return to work after 24 hours with no fever without the use of fever-reducing medication and other symptoms are improving and at least 10 days have passed since symptoms first appeared.
These CDC guidelines for returning to work after a COVID-19 diagnosis may be adapted by state/local health departments to respond to the rapidly changing local circumstances. For specific requirements for returning to work based on your local circumstances, contact your local health department. For specific protocols that a company in the food industry should take if an employee or customer tests positive for COVID-19, visit: https://www.feedingus.org/ or for additional information see: CDC Healthcare Guidelines & CDC Guidelines for Businesses.
Do individuals who are fully vaccinated need to quarantine if they have been exposed to someone with a suspected or confirmed COVID-19 diagnosis?
On February 10, 2021, CDC updated its quarantine recommendations for individuals who are fully vaccinated and have been exposed to someone with a suspected or confirmed COVID-19 diagnosis. Individuals who are fully vaccinated (received the second dose in a 2-dose series) are not required to quarantine following an exposure if they meet all of the following criteria.
- Are fully vaccinated (i.e., ≥2 weeks following receipt of the second dose in a 2-dose series, or ≥2 weeks following receipt of one dose of a single-dose vaccine)
- Are within 3 months following receipt of the last dose in the series
- Have remained asymptomatic since the current COVID-19 exposure
Moreover, it is still important for individuals who are fully vaccinated to continue following CDC’s current guidance in order to protect themselves and others, including wearing a mask, staying at least 6 feet away from others, avoiding crowds, avoiding poorly ventilated spaces, covering coughs and sneezes, washing hands often in additional to following other applicable CDC guidance (e.g., travel, workplace, school guidance, etc.).
Since CDC recommends waiving quarantine for fully vaccinated persons who received their second dose within 3 months, does that mean the vaccine loses its effectiveness after 3 months?
No. Currently, there is limited data available right now. And, although the risk of SARS-CoV-2 transmission from vaccinated persons to others is still uncertain, vaccination has been demonstrated to prevent symptomatic COVID-19; symptomatic and pre-symptomatic transmission is thought to have a greater role in transmission than purely asymptomatic transmission.
CDC’s recommendation to waive quarantine for people who have been vaccinated within 3 months following receipt of the last dose aligns with CDC’s quarantine recommendations for individuals with natural immunity due to having previous infection of COVID-19.
CDC has stated that they plan to update the quarantine recommendations for vaccinated persons, including the criteria for timing since receipt of the last dose in the vaccination series when more data become available and additional COVID-19 vaccines are authorized.
Who needs to wear gloves and when should they wear them?
Personal protective equipment (PPE), such as disposable gloves, are used every day by personnel working in a sector that is a part of the critical infrastructure. COVID-19 has created an increased demand for PPE which has resulted in a shortage of PPE, including gloves. Therefore, it is critical that these essential items only be used when required and should be reserved for people who really need them such as for healthcare personnel who are caring for potentially infectious patients. In retail food establishments, the use of single-use gloves is only required when handling ready-to-eat food and when executing cleaning and sanitation tasks.
According to the CDC, proper hand hygiene, keeping social distance from others and wearing a mask are the most effective ways to prevent the spread of COVID-19. Individuals should practice effective hand hygiene by washing their hands frequently with soap and water for at least 20 seconds.
Employees should avoid bare hand contact with ready-to-eat food by using single-use gloves or another suitable utensil when preparing or serving ready-to-eat food as outlined in Section 3-301.11 of the FDA Food Code. Employees working with ready-to-eat food should wash their hands and the exposed portions of your arms for 20 seconds prior to donning gloves and before touching food or food-contact surfaces. Individuals responsible for cleaning and sanitation should wear disposable gloves for all cleaning tasks to minimize the risk of exposure.
Although gloves are not a substitute for effective hand hygiene, individuals who decide to wear gloves should always wear gloves properly. This includes washing hands prior to donning gloves, removing gloves properly, discarding gloves in the appropriate location and washing hands immediately after removing gloves. Gloves should be changed if the gloves get ripped, torn, or contaminated.
Social Distancing
Regarding crowd size, what recommendations are being put into place?
The CDC released guidance on mass gatherings and COVID-19. The guidance states: “Large events and mass gatherings can contribute to the spread of COVID-19 in the United States via travelers who attend these events and introduce the virus to new communities. Examples of large events and mass gatherings include conferences, festivals, parades, concerts, sporting events, weddings, and other types of assemblies. These events can be planned not only by organizations and communities but also by individuals.”
In accordance with CDC’s guidance for large events and mass gatherings, organizers (whether groups or individuals) should continue to assess, based on current conditions, whether to postpone, cancel, or significantly reduce the number of attendees for gatherings. CDC has provided recommendations for event organizers to consider in order to protect individuals and prevent the spread of coronavirus. Event organizers should work with their local or state health departments to determine what considerations should be implemented depending on the circumstances within their community. Therefore, organizers should check with their state and local governments for more information. Events of any size should only be continued if they can be carried out with adherence to guidelines for protecting vulnerable populations and hand hygiene, wearing a mask and social distancing. When feasible, organizers could modify events to be virtual.
While these recommendations do not apply to sectors identified as being a part of the critical infrastructure, such as the food supply sector, operations can promote distancing by encouraging customers and employees to maintain separation, when possible, from one another to prevent the spread of COVID-19. FMI has developed a customizable signage to promote distancing. Download the Customizable Social Distancing Signage here.
Do grocery stores need to provide dedicated hours for seniors?
Older adults and people with chronic medical conditions are at higher risk of getting sick from COVID-19. CDC recommends that at-risk communities to take precautions to limit close contact with others, avoid crowds and stay home as much as possible due to COVID-19. Offering dedicated shopping hours for seniors is just one example of how the food industry is seeking to support these communities who are at a higher risk for serious illness from COVID-19 by offering safe options to consumers and those shopping on behalf of others.
Other recommendations to help those customers who need assistance in getting their groceries, include:
- Honoring all social distancing protocols, ask a neighbor to add your needed items to their grocery list and arrange a safe means of conducting the necessary transitions.
- Tap a volunteer organization in your county, community, city or state.
- Solicit local faith communities for support.
- Check with your local civic association.
- Be aware that local food banks are working to ensure access as well, such as creating “quarantine kits” for those in need, or “open door” policies so individuals don’t need to touch handles or other entry points in high-touch areas.
For additional information see: CDC Guidelines for Higher Risk Populations.
Do I need to install a plexiglass shield or some other physical barrier at the checkout lane?
To prevent the spread of COVID-19, CDC has recommended that individuals employ social distancing from others, when possible. In retail food establishments, maintaining a full 6 feet distance from another may not always be possible; however, establishments should proactively take action and determine if there are any operational changes that can be made to increase employee separation. Although not required, some companies have installed physical barriers such as plexiglass in an effort to increase separation and prevent the spread of COVID-19. While this may increase the separation between an associate and customer, the risk of transmitting COVID-19 also depends on duration of exposure (i.e., time) and the effectiveness of employee hygiene practices and sanitation. It is important to note that maintaining social distancing in the absence of effective hygiene practices may not prevent the spread of this virus.
To prevent this risk of infection, CDC recommends the following everyday preventive actions:
- Avoid close contact with people who are sick.
- Avoid touching your eyes, nose, and mouth.
- Stay home when you are sick.
- Cover your mouth and nose with a mask when around others
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
- Wash your hands often with soap and water for at least 20 seconds, especially after going to the bathroom; before eating; and after blowing your nose, coughing, or sneezing.
- If soap and water are not readily available, use an alcohol-based hand sanitizer with at least 60% alcohol. Always wash hands with soap and water if hands are visibly dirty.
- Clean AND disinfect frequently touched surfaces
Companies installing plexiglass should comply with all regulations, such as The Americans with Disabilities Act (ADA), along with any state and local requirements.
References
- https://www.cdc.gov/coronavirus/2019-ncov/about/transmission.html
- https://www.cdc.gov/coronavirus/index.html
- https://www.cdc.gov/coronavirus/2019-ncov/about/symptoms.html
- https://www.cdc.gov/coronavirus/2019-ncov/prevent-getting-sick/prevention.html
- https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/coronavirus-disease-2019-covid-19-frequently-asked-questions#food
- https://www.who.int/health-topics/coronavirus
Additional Background Information
- FDA: FAQ on Food Safety and the Coronavirus Disease 2019 (COVID-19)
- CDC: Coronavirus Disease 2019 (COVID-19)
- CDC: Preparing Communities for Potential Spread of COVID-19
- CDC: COVID-19 FAQs
- WHO: Q&A on Coronaviruses (COVID-19)
- Comprehensive And Updated FAQs For Employers On The COVID-19 Coronavirus
- COVID-19 and Food Safety Review FAQ: Is Coronavirus a Concern With Takeout?
Photo credit: "Novel Coronavirus nCoV" by AJC1 is licensed under CC BY-SA 2.0
- Food Safety & Security
 Industry Topics address your specific area of expertise with resources, reports, events and more.
Industry Topics address your specific area of expertise with resources, reports, events and more.
 Our Research covers consumer behavior and retail operation benchmarks so you can make informed business decisions.
Our Research covers consumer behavior and retail operation benchmarks so you can make informed business decisions.
 Events and Education including online and in-person help you advance your food retail career.
Events and Education including online and in-person help you advance your food retail career.
 Food Safety training, resources and guidance that help you create a company food safety culture.
Food Safety training, resources and guidance that help you create a company food safety culture.
 Government Affairs work — federal and state — on the latest food industry policy, regulatory and legislative issues.
Government Affairs work — federal and state — on the latest food industry policy, regulatory and legislative issues.
 Get Involved. From industry awards to newsletters and committees, these resources help you take advantage of your membership.
Get Involved. From industry awards to newsletters and committees, these resources help you take advantage of your membership.
 Best practices, guidance documents, infographics, signage and more for the food industry on the COVID-19 pandemic.
Best practices, guidance documents, infographics, signage and more for the food industry on the COVID-19 pandemic.
